Clinical history:
19 year old male lacrosse player with scrotal pain and swelling after being hit with a lacrosse ballWhat is the diagnosis? (choose all that apply)
- Intratesticular hematoma
- Hematocele
- Testicular fracture
- Testicular rupture
What are potential complications of this condition? (choose all that apply)
- Testicular ischemic necrosis
- Infertility
- Testicular atrophy
- Intratesticular pseudoaneurysm
What are the operative indications? (choose all that apply)
- Rupture of tunica albuginea.
- Large hematocele.
- Large intratesticular hematoma
- Testicular fracture.
Sonographic Findings:
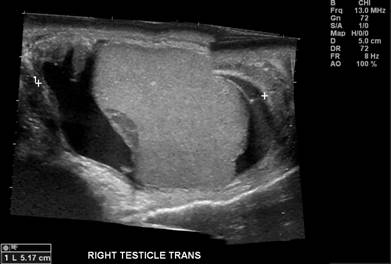
The ultrasound images above demonstrate a complex fluid collection containing low level echoes surrounding the right testis – the appearance is compatible with a large hematocele. There is also discontinuity of the tunica albuginea inferiorly with focal bulging of testicular parenchyma through the tunica albuginea. There is a well-defined hypoechoic area within the right testis that likely represents an intratesticular hematoma. There is normal blood flow within the right testis.
Discussion:
Testicular trauma is a common cause of scrotal pain. The majority of scrotal trauma is blunt trauma. Blunt testicular trauma is usually the result of assault, motor vehicle accidents, or sports-related events. The mechanism of testicular injury in blunt trauma is crushing of the testis against the pubic symphysis or between the thighs. Penetrating and iatrogenic trauma are less common.
Patients will generally present with extreme scrotal pain and nausea. Physical exam reveals varying degrees of swelling and ecchymosis that do not correlate with the severity of testicular injury. In fact, physical exam of the testes is often limited secondary to pain. Scrotal ultrasound is necessary to assess the morphology and vascularity of the testes.
Blunt scrotal trauma can result in testicular rupture, fracture, dislocation or torsion, as well as intra- and extra-testicular hematomas, intratesticular pseudoaneurysms, and hematoceles. Scrotal and epididymal hematomas, epididymal fracture and rupture, and traumatic epididymitis can also occur. An overview of some of these entities follows.
Testicular Rupture
The normal tunica albuginea is a thin echogenic line surrounding the testis. Ultrasound detection of disruption of this structure in a patient with blunt scrotal trauma supports the diagnosis of testicular rupture. Associated findings of a large testicular hematocele, a contour abnormality of the testis, and heterogeneous echotexture of the testis help confirm the diagnosis. Rupture of the tunica albuginea is almost always associated with disruption of the tunica vasculosa which can result is a loss of vascularity to a portion of the testis.
Guichard et al reported a sensitivity of 100% and specificity of 65% for US in the detection of testicular rupture in a series of 33 patients. Another study by Buckley and McAninch demonstrated a sensitivity of 100% and a specificity of 93.5% for the diagnosis of testicular rupture in a series of 65 patients based on ultrasound findings of heterogeneous echotexture of the testis and contour abnormality.
Early surgical exploration and repair of a ruptured tunica albuginea is associated with increased rates of testicular salvage. Testis salvage rates exceed 90% with exploration and repair within 3 days of injury. Complications of conservative management include testicular atrophy, testicular ischemic necrosis, infertility, and delayed orchiectomy. Testis salvage rates with conservative management are approximately 30%.
Testicular Fracture
A testicular fracture refers a break or discontinuity in the normal testicular parenchyma. Ultrasound will demonstrate a linear hypoechoic and avascular fracture line within the testis. The may be seen with or without rupture of the tunica albuginea. Management often consists of debridement along the avascular fracture line while preserving the vascular parenchyma.
Intratesticular Hematoma
These commonly occur in the setting of blunt scrotal trauma. The sonographic appearance of hematomas depends on the time interval between trauma and imaging. Hyperacute and acute hematomas may appear isoechoic or may be heterogeneous. Chronic hematomas appear hypoechoic to anechoic.
Management of intratesticular hematomas largely depends on their size. Small intratesticular hematomas without evidence of rupture or fracture are treated conservatively. Large intratesticular hematomas with or without evidence for fracture or rupture warrant surgical exploration and drainage. Surgery is warranted to relieve elevated intratesticular pressure that can cause ischemic necrosis and testicular atrophy.
Hematocele
This refers to a blood within the layers of the tunica vaginalis, and is the most common finding after blunt scrotal trauma. Its sonographic appearance varies with the age of the hematocele. Acute hematoceles are echogenic, and chronic hematoceles become anechoic over time and develop internal septa and loculations. Chronic hematoceles may become calcified.
Acute onset of large hematoceles may cause reduced blood flow to the testis and may mimic testicular torsion. Large acute hematoceles with or without reduced testicular blood flow require surgical exploration because there may be an underlying testicular rupture. Small hematoceles without evidence of rupture may be managed conservatively.
Antonio Fargiano, M.D.
Department of Radiology
University of Pittsburgh School of Medicine
References:
- S, Dogra VS. Role of US in Testicular and Scrotal Trauma. Radiographics 2008; 28:1617-1629.
- Buckley JC, McAninch JW. Use of Ultrasonography for the Diagnosis of Testicular Injuries in Blunt Scrotal Trauma. J Urol 2006; 175:175-178.
- Deurdulian C, Mittelstaedt CA, et al. US of Acute Scrotal Trauma: Optimal Technique, Imaging Findings, and Management. Radiographics 2007; 27:357-369.
- Guichard G, El Ammari J, Del Coro C, et al. Accuracy of Ultrasonography in Diagnosis of Testicular Rupture After Blunt Scrotal Trauma. Urology 2008; 71: 52-56.
- Micallef M, Ahmad I, et al. Ultrasound features of blunt testicular injury. Injury, Int. J. Care Injured 2001; 32:23-26.
- Wein AJ et al. Campbell-Walsh Urology, 9th ed (2006). Ch 83: Genital and Lower Urinary Tract Trauma. Accessed electronically on March 28, 2009.