Clinical history:
47 year old woman with menorrhagia.
The diagnosis is:
- Myometrial contractions
- Adenomyosis
- Uterine leiomyomas
- Adenomatoid tumor
- Endometrial cancer
Answer: Adenomyosis
Risk factors include (More than one answer may be correct):
- Multiparity
- Nulparity
- Post-menopausal
- Adenomatoid tumor
- Prior uterine surgery (C-section/fibroid resection)
Answer: Risk factors include multiparity.
Treatment options include (More than one answer may be correct):
- Uterine artery embolization
- Endometrial Ablation
- Hysterectomy
- Hormonal suppression
Answer: Treatment options include endometrial ablation, hysterectomy, and hormonal suppression.
Discussion:
Adenomyosis is defined as the deep invasion of endometrial cells into the myometrium, resulting in hypertrophy and hyperplasia of the smooth muscle. The histological appearance is endometrial islands surrounded by hypertrophic, compressed, densely packed smooth muscle cells. Adenomyosis can be further divided into superficial, if confined to the inner 1/3 of the myometrium, or deep if in the outer 1/3. There is no consensus as to the depth of invasion necessary to diagnose adenomysis on histology.2
The pathophysiology is poorly understood, but there are many theories. As adenomyosis is more common in multiparous, premenopausal women, or patients with a history of prior C-sections, trauma to the basal membrane may allow seeding of endometrial cells into the myometrium by direct extension (or through vascular or lymphatic channels). Elevated estrogen levels have also been linked to adenomyosis, and are thought to increase the potential for basalis cells to migrate.3
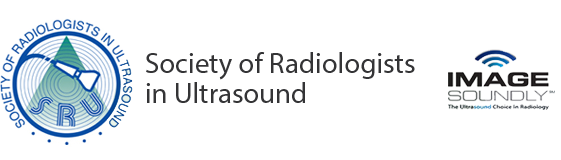
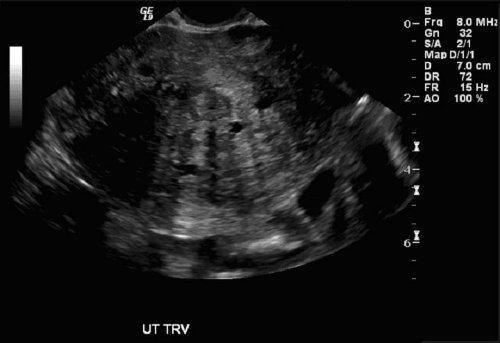
The clinical presentation is commonly menorrhagia, dysmenorrhea, and uterine tenderness. These are the same clinical features seen in many gynecologic conditions, including uterine leiomyomas, so imaging is required for diagnosis. Transvagional ultrasound is the preferred study. The endometrial invasion results in a poorly defined endometrial echo complex. Pseudowidening of the endometrium may be seen. The myometrium appears heterogeneous with hyperechoic islands representing the ectopic endometrial cells, and hypoechoic regions of smooth muscle hyperplasia. Scattered cysts are seen in 40-60% of cases, and represent regions of hemorrhage or dilated glands.2 The uterus becomes diffusely (or asymmetrically) globular in shape, and linear shadowing artifact is often seen (as in this case) due to smooth muscle hypertrophy.2,5,6,7,8
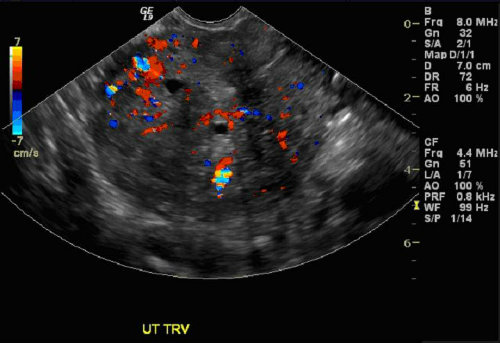
It is important to differentiate adenomyosis from leiomyomas, as the treatment is very different. Leiomyomas can often be conservatively managed with uterine artery embolization, hysteroscopic resection, myomectomy, or high intensity focused ultrasound. Adenomyosis often requires hysterectomy to relieve severe symptoms, although endometrial ablation can be attempted for superficial involvement, and medical management by estrogen suppression is tried in some cases.4 With adenomyosis, there is no mass effect or distortion of uterine contour, as is seen with leiomyomas. Color Doppler imaging would show a peripheral vascular pattern around fibroids, but diffuse vascularity is seen within the myometrium in adenomyosis.1 If the diagnosis is still questionable after ultrasound examination, MRI can be performed to aid in the diagnosis.
Naomi Schwarz, MD
PGY 1, University of Pittsburgh School of Medicine, Department of Radiology
References:
- Chiang CH, Chang MY, Hsu JJ. Tumor vascular pattern and blood low impedance in the differential diagnosis of leiomyoma and adenomyosis by color Doppler sonography. J Assist Reprod Genet. May 1999;16(5):268-75.
- Dueholm, Margit, and Erik Lundorf. “Transvaginal Ultrasound or MRI for Diagnosis of Adenomyosis.” Current Opinion in Obstetrics and Gynecology 19 (2007): 505-12.
- Ferenczy, A. “Pathophysiology of adenomyosis.” Human Reproduction Update 4 (1998): 312-22.
- Levgur, Michael. “Therapeutic options for adenomysosi: a review.” Arch Gynecol Obstet 276 (2007): 1-15.
- Middleton, William D., Alfred B. Kurtz, and Barbara S. Hertzberg. Ultrasound: The Requisites. 2nd ed. St. Louis, MO: Mosby, 2004. 549-50.
- Outwater, Erik K., Evan S. Siegelman, and Vivianna Van Deerlin. “Adenomyosis: Current Concepts and Imaging Considerations.” American Journal of Radiology (1998): 437-41.
- Reinhold C, Tafazoli F, Mehio A, et al. Uterine adenomyosis: endovaginal US and MR imaging features with histopathologic correlation. Radiographics. Oct 1999;19 Spec No:S147-60
- Williams, Penny L., Sherelle L. Laifer-Narin, and Nagesh Ragavendra. “US of Abnormal Uterine Bleeding.” RadioGraphics 23 (2003): 703-18.